Clinical trials are crucial for advancing medical research, but ensuring their integrity and adherence to ethical guidelines is paramount. Good Clinical Practice (GCP) guidelines serve as the backbone, dictating the ethical conduct and quality assurance in these trials. However, violations of these guidelines can occur, leading to various repercussions for both participants and trial outcomes.
What are GCP Violations?
GCP Violations refer to instances where clinical trials deviate from the prescribed guidelines and regulations set forth by international bodies such as the International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) and regulatory agencies like the FDA or EMA. These violations encompass a range of discrepancies that compromise the integrity, validity, and ethical standards of clinical research.
8 Common GCP Violations
Here are 8 most common instances of GCP violations observed in clinical trials.
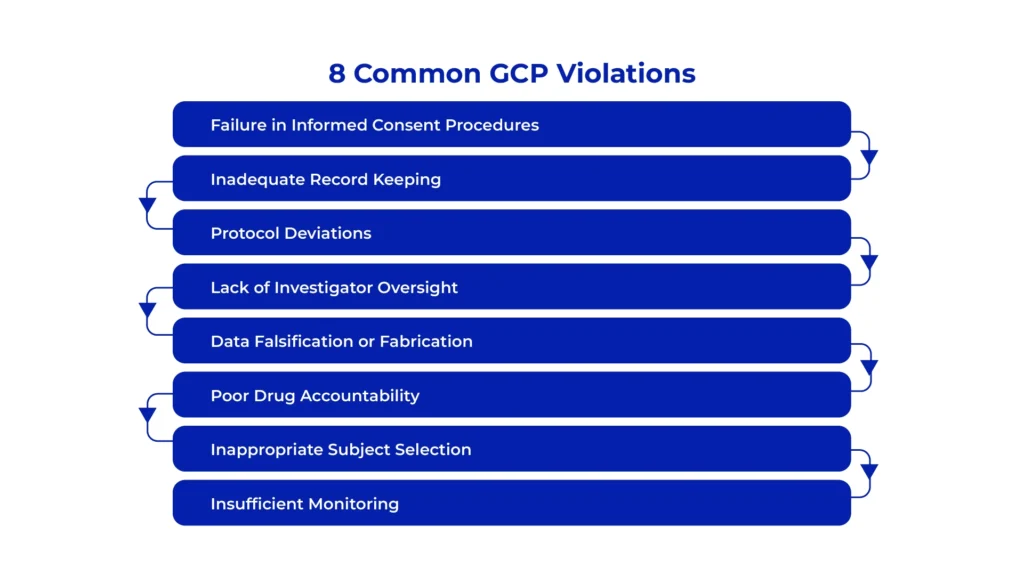
1. Failure in Informed Consent Procedures
Inadequate or improper informed consent processes are a prevalent violation. Participants must fully comprehend the nature of the trial, potential risks, and benefits before enrollment. Failure to provide comprehensive information or ethically obtain informed consent can result in serious breaches.
2. Inadequate Record Keeping
Accurate and comprehensive record-keeping is pivotal in clinical trials. Violations in this aspect, such as missing or falsified documentation, can severely impact the credibility and reliability of trial data.
3. Protocol Deviations
Deviating from the approved research protocol is another common violation. Straying from outlined procedures compromises data accuracy and can undermine the study’s integrity.
4. Lack of Investigator Oversight
Insufficient oversight by investigators can lead to various violations. Lack of supervision might result in poor participant monitoring, incorrect drug administration, or failure to promptly report adverse events.
5. Data Falsification or Fabrication
Perhaps one of the most serious violations, fabricating or falsifying trial data undermines scientific credibility and poses significant risks to participant safety.
6. Poor Drug Accountability
Inadequate monitoring and documentation of investigational drugs, including storage, dispensing, and tracking, can lead to serious compliance issues.
7. Inappropriate Subject Selection
Choosing unsuitable participants for a trial can compromise the study’s validity and the safety of individuals involved.
8. Insufficient Monitoring
Lack of rigorous monitoring throughout the trial duration can lead to unnoticed violations and compromise data integrity.
Impact of GCP Violations
GCP violations have multifaceted impacts, affecting participant safety, trial outcomes, and overall scientific validity. The repercussions extend to regulatory scrutiny, legal actions, and reputational damage for involved parties.
Ways to Prevent GCP Violations
- Preventing GCP violations requires a proactive approach which may involve robust training, stringent quality assurance measures, meticulous monitoring, and clear protocols.
- Examining real-life examples of GCP violations and their consequences sheds light on the seriousness of non-compliance and its implications. This would help the organizations to know about the do’s and don’ts in clinical trials, which would help them to avoid GCP violations.
- Enforcing strict actions and penalties for GCP violations by Regulatory bodies helps to maintain ethical standards and ensure compliance by companies during their clinical trials.
Conclusion
Ensuring adherence to GCP guidelines is imperative in conducting ethical and reliable clinical trials. Straying from these principles not only risks participant safety but also undermines the validity and credibility of scientific advancements.
Upholding Good Clinical Practices remains central to the responsible and impactful progression of medical research. Only by abiding by these practices can we really foster safety and have assured success.